Intoeing
Intoeing: Its not a diagnosis!! It’s just a peculiar pattern of walking which is noticed by the family. It is important that the treating doctor identifies the specific cause for the intoeing . So in scientific terms an intoeing gait pattern is unilateral or bilateral internal rotation of the long axis of the foot to the line of progression (the direction in which the child is moving)( Figure 1)

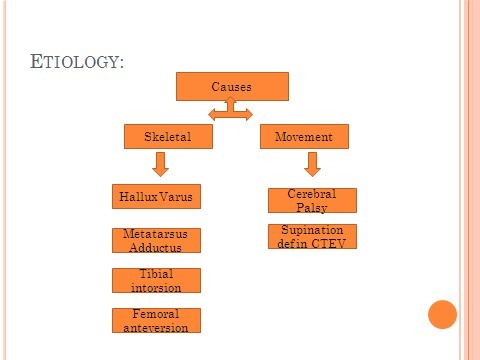
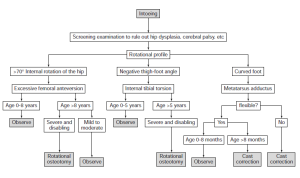
Causes: There are various causes which lead to intoeing. Broadly they can be divided in skeletal causes: Foot-Hallux varus or metatarsus adductus, tibia- Increased intorsion, femur- increased anteversion or a combination) and movement causes(Neuromuscular disorders, dynamic supination in clubfoot) (Figure 2)
Evaluation: Since its important to identify the underlying cause, a through evaluation is needed.
History: Brief birth history to identify any perinatal cause for neurological disorders. Milestones: Age of walking, pattern of walking and sitting, esp “W” sitting (Figure 3). Is the intoeing worsening or improving? Does it affect the function of the child- frequent falls?
Examination: First and foremost, patiently observe the Gait of the child. While walking note the position of the foot, the foot progression angle and the position of the patella. In prone position,perform Staheli’s rotational profile examination:Femur – Flex the knee to 90 degrees, evaluate hip range of motion (internal andexternal rotation) and femoral anteversion. Tibia – View foot and thigh from above and evaluate the long axis of the footrelative to the thigh(Thigh –foot angle). Feet – Does the foot have a straight lateral border, or is it curved/bean shaped?With metatarsus adductus, which is associated with intrauterine positioning,the forefoot is curved inward compared to the hindfoot. Hallux varus will have a bend from the metatarsophalangeal joint.
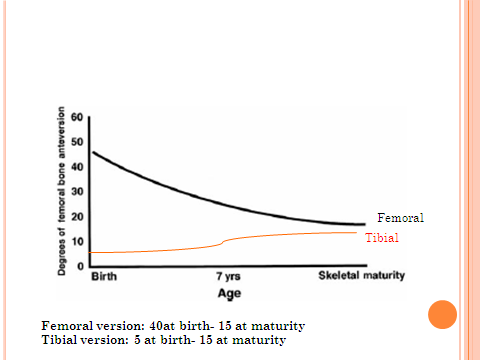
Growth Variation: Femoral anteversion is approximately 40 degrees in newborns, and approximately 15 degrees at maturity. The tibia is mildly internal in toddlers
(-20 to -10 degrees), neutral for children 3-5 years old, and mildly external in children older than 5 years (0 to +15 degrees).(Figure 4)
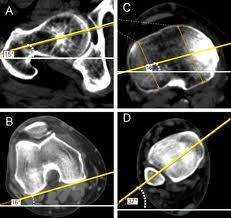
Investigations: Radiographs: Do not have a much role, except for a Pelvis Anteropoasterior view shows Coxa valga in presence of increased femoral anteversion. Special views and conversion: Not practical in day to day practice. CT Scan: Best imaging and investigation for evaluation of the version( Figure 5)
Treatment: No role of special shoes, wedges/insoles, casts, Braces or splints.
So, Is surgical intervention actually needed?? Natural history studies reveal that Spontaneous Resolution occurs in 80% of these children. Residual deformities have not been shown to affect running, jumping, or risk of future arthritis. The best course is to explain the anticipated natural progression of the child’s alignment to the family and reassurance continues to be the recommended initial responses to intoeing in children.
Choice of Procedure: Proximal femoral derotation osteotomy for correction of femoral anteversion and for tibial version correction is supramalleolar tibial derotation osteotomy (Figure 6)
The indications for correction of femoral version are: (Staheli et al JBJS Am;1985):
- Persistence of deformity after 8 years of age
- Functional and cosmetic disability
- Anteversion >50
- Deformity >3SD above the Mean
Indications for correction of tibial version are:
- Deformity persistent after age 5 years
- Functional or cosmetic disability
Neuromuscular Disorders need treatment for the correction of version.
Article Written by – Dr Chasanal Rathod